Often referred to as "wear-and-tear arthritis," osteoarthritis is a prevalent condition that typically arises with aging. While it can affect any joint, it most commonly impacts weight-bearing joints like the hip.
Hip osteoarthritis leads to pain and stiffness, making everyday tasks such as bending to tie shoes, standing up from a chair, or walking short distances challenging.
As osteoarthritis progresses gradually, early treatment is essential to minimize its effects on daily life. While there is no cure, various treatments can help manage pain and maintain mobility.
Hip Anatomy
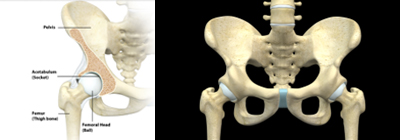
The hip joint is among the largest joints in the body, classified as a ball-and-socket joint:
- The socket is part of the acetabulum, which is located within the pelvic bone.
- The ball is the femoral head, the upper portion of the thighbone (femur).
The surfaces of the ball and socket are covered with articular cartilage, a smooth, slippery material that cushions the bones and ensures easy movement.
The joint's surface is lined by the synovium, which produces fluid to lubricate the cartilage and aid in seamless joint movement.
What is Osteoarthritis of the Hip?

Osteoarthritis is a degenerative condition that typically affects individuals over 50 but can also occur in younger people.
In osteoarthritis of the hip, cartilage in the joint wears down over time, becoming rough and frayed. This deterioration reduces the protective joint space, causing bones to rub together. To compensate, the body may develop bone spurs (osteophytes), which can further contribute to discomfort and restricted motion.
The disease progresses slowly, and pain tends to worsen over time.
Causes of Hip Osteoarthritis
Although osteoarthritis doesn’t have a singular cause, several factors increase the risk of developing the condition:
- Advancing age
- A family history of osteoarthritis
- Previous hip injuries
- Obesity
- Hip joint abnormalities present at birth, such as developmental dysplasia
It’s also possible to develop osteoarthritis without any of these risk factors.
Symptoms of Hip Osteoarthritis
The primary symptom of hip osteoarthritis is pain, which develops gradually and worsens with time, though it may occasionally begin suddenly. Other common symptoms include:
- Pain in the groin or thigh that radiates to the buttocks or knee
- Discomfort that worsens after intense physical activity
- Stiffness, particularly after periods of inactivity or in the morning
- A grinding or "locking" sensation in the joint, caused by loose cartilage fragments
- Reduced range of motion, leading to difficulty walking or a noticeable limp
- Sensitivity to changes in weather, with increased joint pain on rainy days
How is Osteoarthritis of the Hip Diagnosed?
During an evaluation, your doctor will discuss your symptoms, medical history, and conduct a physical exam, which may include diagnostic imaging like X-rays.
Physical Examination
Dr. Avino will check for:
- Tenderness around the hip
- Range of motion (both assisted and unassisted)
- Crepitus, a grating sensation in the joint
- Pain under pressure on the hip
- Gait issues and signs of muscle or ligament damage
Imaging Tests
- X-rays: Provide detailed views of bones, often revealing joint space narrowing, bone changes, and osteophytes.
- MRI or CT scans: Sometimes used to examine soft tissues and bone in greater detail.
Treatment Options for Osteoarthritis of the Hip
Though osteoarthritis cannot be cured, treatments are available to reduce pain and improve mobility.
Nonsurgical Treatments:
Lifestyle Modifications:
- Avoid activities that strain the hip, such as stair climbing.
- Opt for low-impact exercises like swimming or cycling.
- Lose weight to relieve stress on the joint.
Physical Therapy: Exercise programs can improve flexibility, strengthen hip and leg muscles, and enhance range of motion.
Assistive Devices: Using tools like canes or walkers can improve mobility, while devices like reachers can help avoid painful movements.
Medications:
- Over-the-counter pain relievers like acetaminophen (Tylenol) for mild pain.
- NSAIDs, such as ibuprofen, for pain and inflammation.
- Corticosteroids, administered orally or by injection, to reduce inflammation.
Surgical Treatments:
Surgery may be recommended if nonsurgical approaches fail to relieve pain and restore mobility.
Total Hip Replacement: Both the acetabulum and femoral head are replaced with artificial components made of metal, plastic, or ceramic.
Hip Resurfacing: This procedure caps the femoral head with a smooth metal cover, leaving more bone intact compared to a total replacement.
Osteotomy: Rarely used, this procedure realigns the bones to reduce joint pressure.
Potential Complications
Complications like infection, blood clots, or hip dislocation can occur, but doctors take measures to minimize risks.
Recovery
Recovery after hip surgery varies depending on the procedure but often involves physical therapy to restore motion and strength. Temporary use of mobility aids may also be necessary.
Most patients experience significant pain relief and improved daily function after surgery.









